Transgender and non-binary patients are started on gender-affirming hormone therapy (GAHT) in a range of primary and secondary care settings, but ongoing management of prescriptions is by GPs.
GAHT prescribing follows the Guidelines for Gender Affirming Healthcare for Gender Diverse and Transgender Children, Young People and Adults in Aotearoa, New Zealand.
This MedCase considers how GPs can safely provide repeat prescriptions for patients who have already commenced gender-affirming hormone therapy.
It covers the medications funded by PHARMAC at the date of publication.
How is GAHT usually started?
Pathways to starting GAHT vary between DHB's. Most commonly, it is commenced by endocrinology or sexual health, with a gradually increasing number of GPs coming on board to commence hormones under an informed consent model in primary care.
Many secondary care services require a readiness for hormone assessment by a mental health professional before starting hormones. Following this, a thorough consent process outlining permanent and reversible effects and discussion of risks is undertaken.
Testosterone (masculinising) hormones
This section looks at how GPs can safely provide repeat prescriptions for patients who have already been commenced on testosterone based/masculinising gender-affirming hormone therapy (T-GAHT).
What medications are used for T-GAHT?
There are three routes of testosterone administration used in NZ. Most people choose injections due to the less frequent dosing and more stable hormone levels.
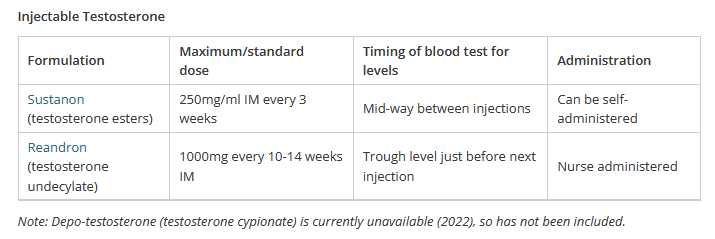
Oral Testosterone: Andriol capsules are not currently funded unless someone is already on them. Due to frequent dosing required for stable levels, and the risk of liver toxicity, these are not as commonly used for GAHT.
Topical Testosterone: Androderm patches 7.5mg daily (skin irritation is common).
Sam is a 20-year-old transgender male who was started on testosterone injections by the endocrinology clinic 2 years ago.
He requests a repeat prescription online. His last prescription was for Reandron 1000mg every 3 months given by IM injection.
Although he comes to see the nurse for his injection every 3 months, you don't know him well, and he last attended a GP appointment over a year ago.
What do you need to consider before repeating his prescription?
Renewing a T-GAHT prescription
Once a person is on standard doses of testosterone, there are not usually many changes to their prescription, however, some people may wish to increase more gradually, and these people may require up-titration of their dose. They require 3-6 monthly blood tests (see below) in the first year and annually thereafter. It is recommended to monitor their BP and weight annually.
You may wish to review your patient to check in with how they are going, in particular:
- Are they happy with the testosterone and the effects they have experienced?
- Are they experiencing any side effects or problems they wish to discuss?
- Do they want to continue taking testosterone?
- Are any other referrals for gender-affirming healthcare required?
You decide to ask Sam to book an appointment so that you can catch up with him and check how the testosterone is going for him.
You review Sam's notes and see that his BP was normal 3 months ago when the nurse checked it at his last injection. Sam's last blood test was over a year ago and, at that time, was normal.
Do you need to arrange any monitoring for Sam, and if so, what do you request?
Monitoring
Blood tests should be checked 3-6 monthly in the first year and annually thereafter.
| Investigation | Comment |
| Complete blood count | If the haematocrit > 0.52, reduce the dose of testosterone and/or discuss with an endocrinologist or haematologist |
| Liver function tests | |
| Lipids | Follow NHF CVD guide consider as for male |
| Testosterone |
|
Testosterone dose can be adjusted by the GP as needed to ensure suitable levels, as long as the recommended maximum dose is not exceeded.
Common questions
Low dose testosterone
Some people (such as non-binary patients) prefer to take low dose testosterone. They should be informed that the same permanent effects as someone taking standard doses are likely to occur. People may wish to start on a low dose and increase more slowly, or they may choose to remain on a low dose.
There is little evidence to guide practice, but many experts recommend maintaining testosterone of >5-6 nmol/L to reduce longer-term cardiovascular or bone risks. Testosterone dose can be adjusted as per patient’s wishes, provided adequate testosterone levels for bone health are maintained and that maximum doses are not exceeded.
Vaginal bleeding
Monthly bleeding will stop in most individuals after 3-6 months on testosterone but may continue in around 10%. Progesterone can be used to stop periods, and if contraception is also needed, this could be in the form of a Mirena, Depo-Provera or a combined/progesterone-only oral contraceptive.
For new-onset bleeding, check that testosterone levels are in the normal range, and if so, investigate as per usual guidelines.
Other considerations
- Ensure you have recorded the patient's desired name and pronouns on your PMS.
- Anyone with a cervix requires cervical screening – ensure recalls are not missed.
- If indicated, contraception is needed even if periods have stopped.
- Many trans masculine patients use a binder. This can cause discomfort or breathing issues for which physiotherapy is useful.
- Gender affirming genital surgery referrals can be made after 12 months of hormone therapy. Referral informarion can be found here.
Oestrogen based (feminising) hormones
This section looks at how GPs can safely provide repeat prescriptions for patients who have already been commenced on oestrogen based/feminising gender-affirming hormone therapy (E-GAHT).
What medications are used for E-GAHT?
A testosterone blocker and oestrogen are required, with neither fully effective in isolation.
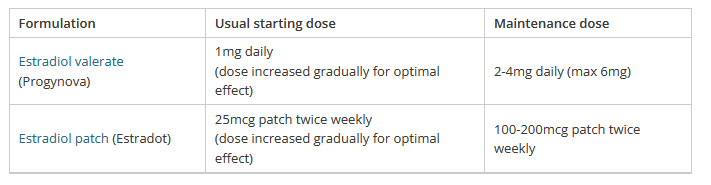
Oestrogen
The funded formulations of oestrogen are transdermal patches or oral tablets. Patches may be preferable due to a lower thromboembolic risk. Transdermal oestrogen avoids liver metabolism, so is also the preferred choice if there is any liver function impairment.
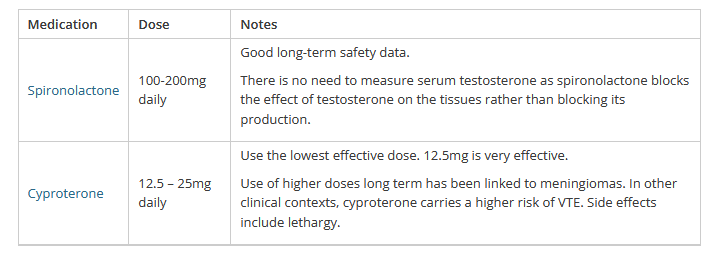
Testosterone blocker
There is a choice of two as per the table below. Choice of blocker may depend on prescriber or patient preference. If the patient has an orchiectomy, the blocker can be stopped.
Bella is a 32-year-old transgender woman who was started on gender-affirming hormone therapy ten years ago by the endocrinology clinic.
She is new to your practice, and you have not provided a repeat prescription for her before.
Bella requests a prescription for her usual medication, which is listed as progynova 5mg and cyproterone 50mg. You cannot see any recent blood test results.
What do you need to consider before repeating her prescription?
Renewing an E-GAHT prescription
Once someone is well established on GAHT, you may wish to see them once a year to:
- Check they are happy with their hormones and the effects.
- Address any questions, concerns or side effects.
- Ensure BP and blood test monitoring is up to date
- Check if any referrals for other gender-affirming care are required.
You ask Bella to come in for an appointment so that you can meet her, check her blood pressure and discuss her medications.
Bella has a normal BP and is happy with the effects of the hormone therapy.
You let Bella know that current recommendations are to use the lowest effective dose of cyproterone and that her dose can be reduced. She is a little wary of making changes but agrees to reduce the cyproterone to 25mg od with a view to further reducing in the future if that goes well.
You ask Bella to go for a blood test as this hasn't been done in the last 12 months. Which blood tests do you check?
Monitoring
Blood tests should be checked 3-6 monthly in the first year and annually thereafter.
Monitoring blood tests for a patient on oestrogen-based GAHT:
| Investigation | Comment |
| Electrolytes | If on spironolactone |
| Liver Function Test | If abnormal use transdermal oestrogen and avoid cyproterone |
| Lipids | Treat according to NHF CVD guide – consider as a male (conservative option) |
| Oestrogen | Only checked to ensure levels aren't supraphysiological. There is no target level as evidence suggests that levels don't correlate with physical effects, and exogenous oestrogen is not well measured in the serum. Oestrogen level should not exceed 500pmol/L |
| Testosterone |
On cyproterone – level should be suppressed <2nmol/L On spironolactone – no need to measure as it doesn't usually suppress |
Bella's results are normal, and you provide her with a 3 month prescription for progynova 5mg od and cyproterone 25mg od, with a plan to see her in 3 months to discuss a further cyproterone reduction.
Common questions
Cardiovascular risk
In someone with risk factors for thrombosis and increased cardiovascular risk (e.g. smoking, IHD, migraine with aura, older age), it's recommended to use oestrogen patches at the lowest effective dose, and a discussion about the potential risk of cyproterone is warranted.
There is limited data available, but given the increased VTE risk when using cyproterone in other contexts (e.g. GINET), this would seem sensible.
Patients need to be informed of the risk of oestrogen increasing the risk of thrombosis and CVD, but it would be unethical to withhold treatment. The benefits of GAHT (and the risks of withholding it) need to be weighed against any potential increased risk.
Progesterone
Some clients may request progesterone treatment, particularly to support breast development. At present, there is no good quality evidence to support an effect, and it may increase the risk of venous thromboembolism. Therefore, most guidelines, including the NZ guidelines, recommend against its use as part of feminising GAHT.
Other considerations
- Ensure you have recorded the patient's desired name and pronouns on your PMS.
- Feminising GAHT causes infertility, and patients should have been offered fertility preservation before starting GAHT.
- Gender affirming voice therapy is available in some regions
- Gender affirming genital surgery referrals can be made after 12 months of hormone therapy. The referral form can be found here.
This MedCase was written in 2022 by Dr Rona Carroll ( she/her), Senior Lecturer University of Otago and General Practitioner and reviewed by Professor Bruce Arroll, University of Auckland.
Supported by
Recognition of Learning Activities
Don't forget to log your time with The Royal New Zealand College of General Practitioners portal for recognition of learning activities.