This MedCase was first published in January 2020. It was updated by Dr Hazel Fuiava, MBChB, Dip Paeds, FRNZCGP.
Evaluating driving safety in patients with mild cognitive impairment (MCI) or dementia can be challenging as there is no single marker that determines fitness to drive.
This MedCase discusses driving assessment for a patient with mild dementia using Medical Aspects of Fitness to Drive (2024) and Dementia and Driving Safety: A Clinical Guideline (2014).
Mr R is a 73 year old Māori man who comes with his wife to discuss a recent diagnosis of dementia made by the specialist memory clinic. He scored 72/100 on the Addenbrooke’s Cognitive Examination (ACE) III assessment. Blood tests and a CT head showed no underlying cause for dementia.
You have known Mr and Mrs R for many years. Mr R has hyperlipidaemia, type II diabetes, and hypertension, which are adequately controlled on his regular medications: atorvastatin 40mg nocte, metformin 1000mg twice daily, and losartan 50mg.
Mr R is a retired fisherman who now works part-time as a handyman at the primary school, where Mrs R works part-time as a teacher aide.
You notice that Mr R drove them to today’s appointment. What do you do now? Do you need to assess Mr R’s ability to drive?
When to assess?
A diagnosis of MCI or dementia is not necessarily a reason to stop driving, but should trigger an assessment of driving safety, since any cognitive impairment can be associated with greater risk of accidents or near-misses.1
The risk increases with dementia severity, as shown in the table below from the Dementia and Driving clinical guideline.1
Additionally, many patients with dementia have comorbidities or take medications that further impact their driving safety.3 Age is also a consideration: older drivers are second only to the youngest drivers in terms of crash risk.
| Dementia stage | Driving recommendation |
| No dementia | May continue to drive Check for other medical conditions. |
| Mild cognitive impairment | Most people safe to drive. Consider occupational therapy (OT) driving assessment, restricting or stopping driving if:
Notify NZTA |
| Mild dementia | Driving safety is uncertain:
Person needs further investigation / review:
Clinical decision needs to be made:
|
| Moderate dementia | Must stop driving Notify NZTA |
| Severe dementia | Must stop driving Notify NZTA |
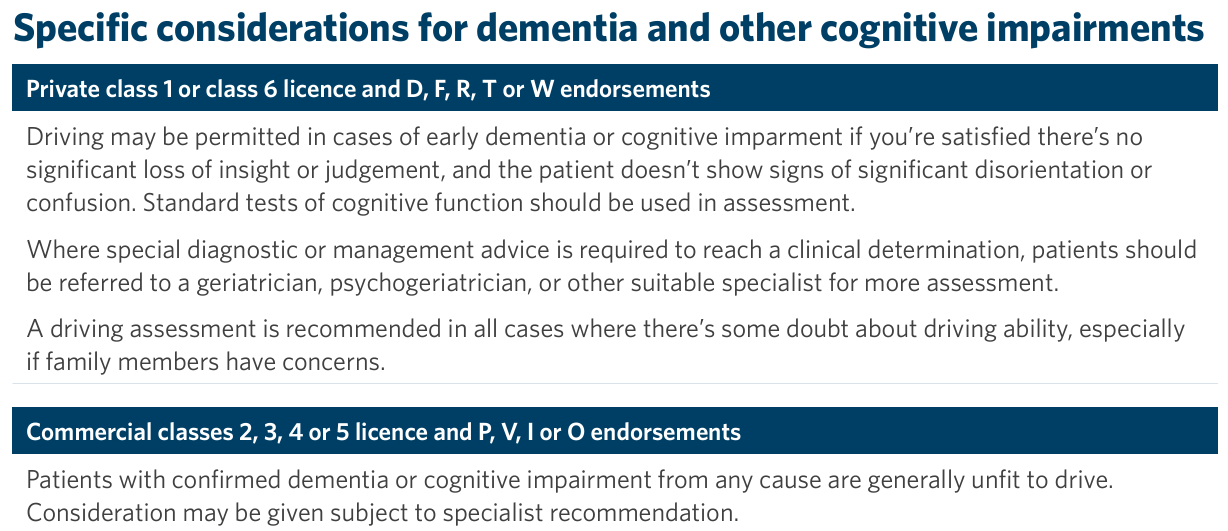
Safety to drive in dementia also depends on the license classes and endorsements held. These considerations are summarised in the updated Medical Aspects of Fitness to Drive manual, chapter on Dementia:
Practice points: Discussing driving and dementia
Explain to patients and their families that:
- There is a clear link between dementia and driving safety.
- Driving safety assessment will be a regular part of clinical review.
- Patients will eventually need to stop driving (as dementia progresses).
- Patients must advise their insurance company about conditions such as dementia that are likely to affect driving.
Useful patient resources:
- Dementia and driving Waka Kotahi NZTA
- Alzheimer’s New Zealand driving section
- Dementia and driving Healthify
How to assess fitness to drive in patients with dementia
This decision is more straightforward in cases of moderate or severe dementia, when driving must be stopped, but is more difficult in cases of mild dementia or MCI, as safety cannot be inferred from cognitive test results or dementia stage. Clinical assessment is required. A thorough assessment is likely to require two visits along with collateral history from family members.
You raise the topic of driving and explain the link between memory impairment and unsafe driving.
Mr R is initially reluctant to have an assessment, as he lives rurally and there are no buses or regular taxi services nearby.
You explain that you understand the significant consequences of being unable to drive, but that you are required by law to ensure that Mr R is safe on the road. With some encouragement from Mrs R, Mr R consents to an assessment.
You suggest that you begin the assessment today, but that a second visit will likely be required before you can make a decision.
Initial assessment
The first assessment should use readily available information to assess driving safety. Some things to consider:
- Understand how the patient and their family members (if present) feel about their driving, including asking about accidents or near-misses, and overall function.
- Cognitive test score (repeated if not completed one recently).
- Review comorbidities and medications that may affect driving safety, including alcohol.
- What is the practical impact of losing a driving licence? Are there other drivers in the household? What alternatives are available?
You review Mr R’s comorbidities and medications. He has well-controlled diabetes and hypertension and is not taking any other medications that may impair his driving ability. He drinks 1-2 cans of beer on 3-4 nights of the week.
Next, you ask Mr R about his driving. He admits that he has been restricting his driving to short daytime trips lately, mainly to the local town to get his newspaper and Lotto ticket. Mrs R drives if a longer journey is necessary. He has had a recent near-miss while reversing in a car park in town, but no accidents in the past few years.
You explain to Mr R that you can’t make a decision about his driving today as you need more information.
Second assessment
It may be possible to make an assessment about driving safety after reviewing readily available information, but if not then further specific investigations are required.
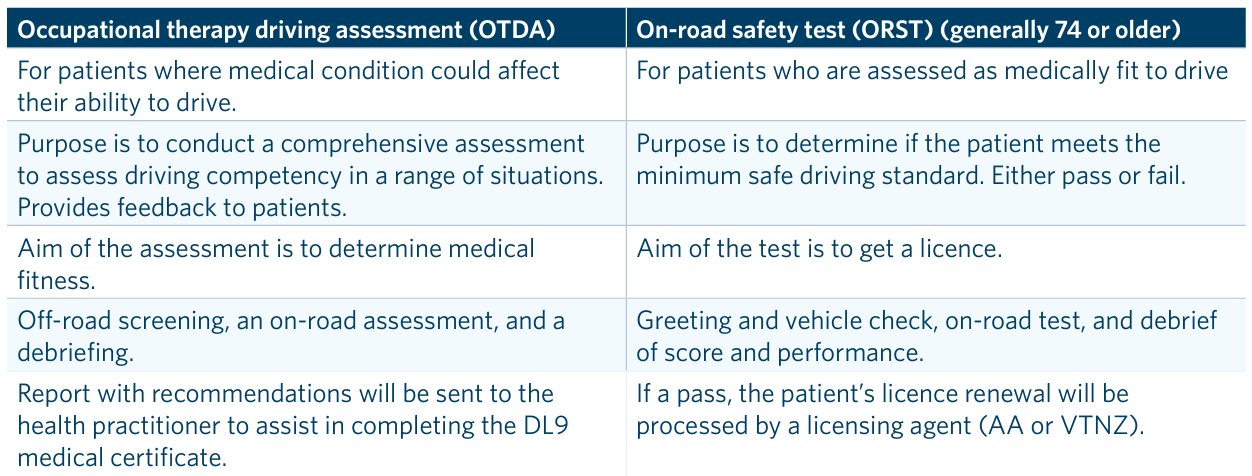
The Occupational Therapy Driving Assessment remains the most rigorous and reliable test of driving safety, and it is the only test that allows clinical input from referrers to inform the OT decision. However, the cost of over $500 is prohibitive for many patients.
If patients are unwilling or unable to undergo an OT assessment, then clinicians must rely on other sources of information, such as:
- Other on-road assessments, such as those run by local driving schools. Note that the AA Senior Driver programme is a preparation test rather than an assessment, but it can provide useful information to support clinical judgement.
- Collateral information from whānau, for example using a Driving Questionnaire (from p33, Dementia and Driving Safety guideline).
- Further cognitive or functional testing (see Table 3, p17, Dementia and Driving Safety guideline for suggestions).
- Consider referring to a secondary care team for specific driving assessment.
There is a useful summary of practical driving assessments (page 17) in Medical Aspects of Fitness to Drive.
You discuss options for further testing with Mr R.
He is unable to pay for an OT Driving Assessment and he is not an AA member.
In the absence of on-road driving information, you offer a family meeting with his whānau next week to discuss driving, and he agrees to bring along his two daughters.
Whakawhānaungatanga: Ensuring good outcomes for Māori patients with dementia
The concept of whakawhānaungatanga involves building connections and sharing information. It is part of The Hui Process,4 a four-step approach to relationship building with Māori patients and their whānau that involves:
- Mihimihi (introductions)
- Whakawhānaungatanga (building connections and sharing information)
- Kaupapa (discussing the main issues)
- Poroporoaki (closing the interview and ensuring shared understanding).
When used effectively, the Hui Process can help ensure a safe and appropriate decision is made about driving. Take time to understand who should be involved in driving assessment and offer a family meeting if necessary.
Mr R’s wife drives Mr R and their two daughters to your practice one week later for a half-hour meeting. Your existing relationship with Mr and Mrs R means that the mihimihi and whakawhanaungatanga steps are well established with them, but for the benefit of their two daughters you introduce yourself (mihimihi) and share some stories about your background growing up in the country (whakawhanaungatanga).
Mr R’s two daughters introduce themselves. They tell you they see their father regularly and are pleased to be included in this meeting, as they weren’t able to attend the hospital appointment when he was diagnosed with dementia.
Next, you move on to the kaupapa phase: driving safety. You reiterate the link between dementia and driving safety, and ask the whānau for their thoughts. Mrs R tells you that they have already made some changes due to concerns about Mr R’s driving. For example, Mrs R is now the driver for long distances and at night, because they noticed that Mr R became tired and began driving very slowly.
Their daughters raised concerns about Mr R becoming confused with the mokopuna in the car; he once drove them to the wrong house after kohanga. They prefer Mrs R to drive the mokopuna.
Mr R concedes he gets tired driving long distances and says he has become confused on a few occasions in town where it is busy and he feels pressured. He is happy to be driven into town, but wants to keep his licence so that he can visit his friend’s farm two kilometres away, where he likes to go a few times each week for a cup of tea. The whānau feel that this is probably safe.
You reach agreement on a plan for Mr R to limit driving to within 5 kilometres from home, during the daytime. You will notify NZTA of the new restrictions.
You agree to review driving safety in 6 months, or earlier if there are any new concerns.
In closing, you congratulate Mr R on a successful driving career. Mr R tells you that he will be happy to stop driving eventually and may even do this before he sees you next, but he is pleased to have his licence for now.
Outcomes and review
There are three possible outcomes from a driving assessment:
- continue to drive for the moment
- continue to drive with certain limitations, e.g. time of day and/or local area only
- stop driving.
If the patient continues driving, a review must be planned. It is important to highlight to patients that eventually they will need to stop driving altogether.
Practice points
- There is a clear link between dementia and unsafe driving.
- Many patients with MCI or mild dementia will be safe to drive, but cognitive test scores are not useful predictors in these groups and thorough clinical assessment is required.
- An on-road OT Driving Assessment remains the best test where possible.
- Consider further cognitive testing, driving questionnaires, and family meetings for collateral history when an on-road assessment is not possible.
- If the patient is safe to drive, a planned review must be scheduled.
- Educate all patients with dementia that eventually they must stop driving.
This MedCase was created in January 2020 by Dr Vicki Mount, General Practitioner, MBChB, DipPaeds, with expert review from Dr Philip Wood, Geriatrician, MBChB, FRACP.
Supported by
Recognition of Learning Activities
Don't forget to log your time with The Royal New Zealand College of General Practitioners portal for recognition of learning activities.